

Kai Institute is Preserving Culture Through Kai
Published date : Mon, 18 March 2024 10:28 AMA movement that is dedicated to re-introducing traditional kai practice, preserving kai mātauranga (knowledge) and protecting the cultural identity of Māori.


Nursing Degree offered in Wairoa
Published date : Tue, 27 February 2024 03:58 PMTe Whare Wānanga o Awanuiārangi is now delivering Nursing course in Wairoa.
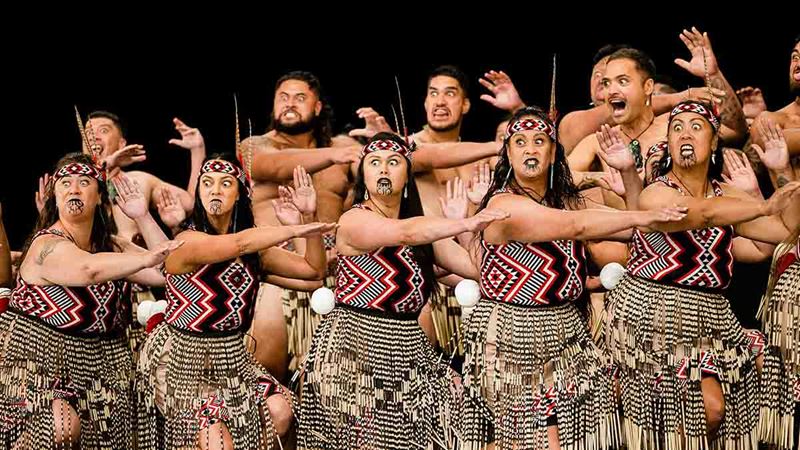

Te Whānau a Apanui to defend Mataatua title 2024
Published date : Sat, 24 February 2024 07:00 AMTe Kapa Haka o Te Whānau a Apanui will be defending their Mataatua Regionals title this year and they share insights to their long-standing relationship with Te Whare Wānanga o Awanuiārangi.
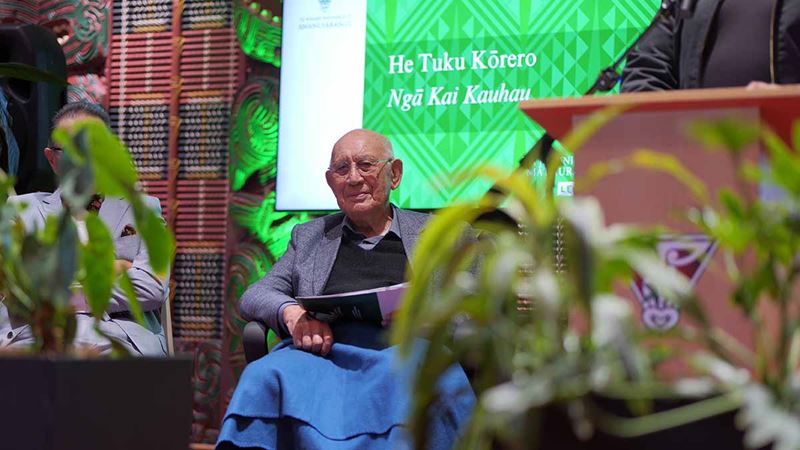

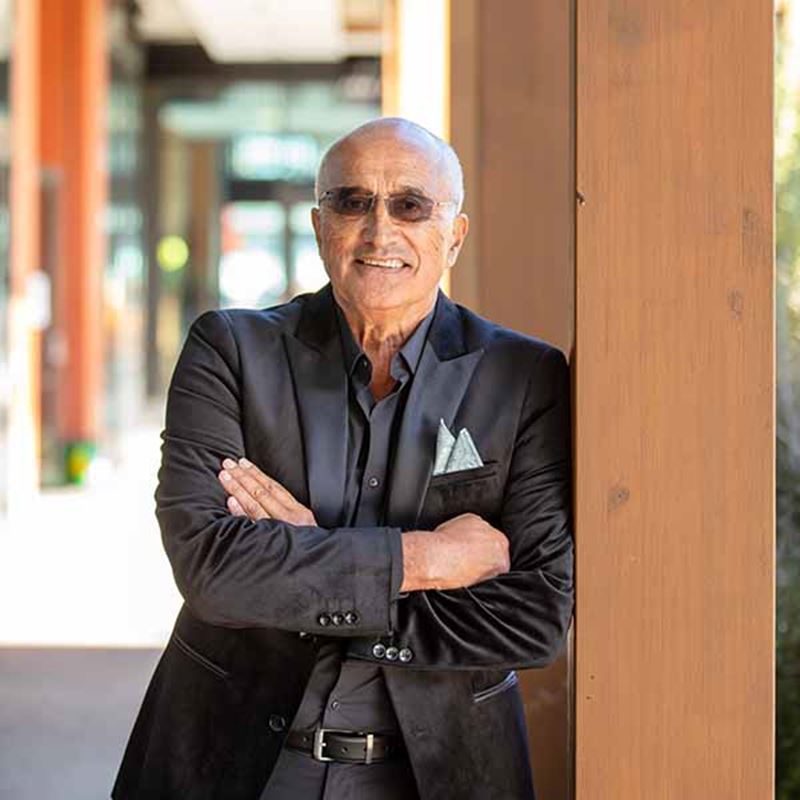
Tā Hirini Moko Mead Receives Award
Published date : Tue, 20 February 2024 04:00 PMTā Hirini Moko Mead honored with Te Whare Pukenga Award

Supporting Mataatua Kapa Haka Regional Competition 2024
Published date : Tue, 20 February 2024 01:00 PMTe Whare Wānanga o Awanuiārangi is a proud sponsor of the Mataatua Kapa Haka Regionals 2024.
Awanuiārangi Professor Shines a Spotlight on Legislative Redress and Historical Discourse
Published date : Fri, 02 February 2024 01:00 PMAwanuiārangi Professor Shines a Spotlight on Legislative Redress and Historical Discourse


New Māori Health Scholarship Te Rau Wānanga
Published date : Fri, 26 January 2024 12:16 PMTe Whare Wānanga o Awanuiārangi in partnership with Te Aka Whaiora are offering a new scholarship for students with a commitment to contributing to Māori Health.


Nursing Pinning Ceremony
Published date : Tue, 16 January 2024 11:33 AMAwanuiārangi Celebrates Resilience and Commitment at Nursing Pinning Ceremony

New Bachelor of Education Programme
Published date : Mon, 15 January 2024 03:58 PMNew Bachelor of Education Programme Receives Commendations in NZQA Teaching Council Review


Wānanga takes Kura Reo across the Tasman
Published date : Wed, 06 December 2023 12:10 PMTe Whare Wānanga o Awanuiārangi offers Te Pōkaitahi Reo to tauira in Australia for the first time